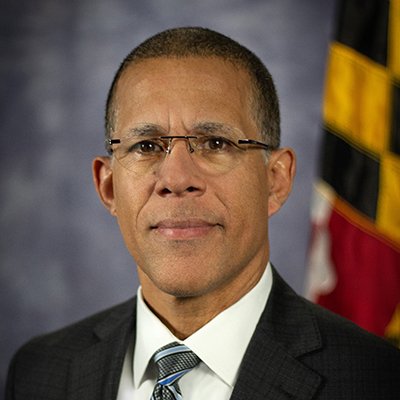
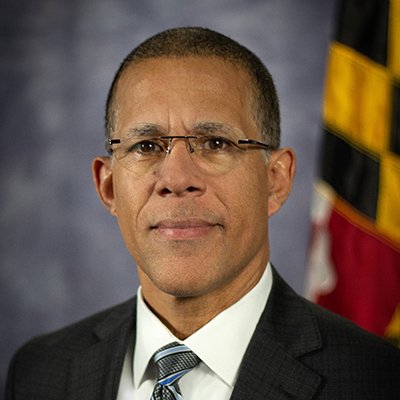
Attorney General Anthony Brown joined a multistate lawsuit challenging a new federal rule by the Trump administration that would modify Affordable Care Act regulations, potentially leading to insurance loss and increased costs for millions, including 34,000 Marylanders.
Per the news release distributed on Thursday, July 17: “Attorney General Anthony G. Brown today joined a multistate coalition in filing a lawsuit challenging an unlawful final rule promulgated by the U.S. Department of Health and Human Services (HHS) and Centers for Medicare & Medicaid Services (CMS) that would create significant barriers to obtaining healthcare coverage under the Affordable Care Act (ACA).
The Trump administration’s final rule would make numerous changes to rules governing federal and state health insurance marketplaces. Trump’s own administration estimates the changes will cause up to 1.8 million people to lose their health insurance, while causing millions more to pay increased insurance premiums and out-of-pocket costs like copays and deductibles. The final rule also excludes coverage of gender-affirming care as an essential health benefit (EHB) under the ACA.
“The 34,000 Marylanders who stand to lose their insurance because of this new policy won’t just lose health coverage – they’ll lose access to cancer screenings, blood pressure medications, and chemotherapy treatments that could save their lives,” said Attorney General Anthony Brown. “We’re filing this lawsuit because the Maryland Health Benefit Exchange has helped thousands of families improve and protect their health, and we will not let the Trump administration strip Marylanders of the coverage and care they rely on—or force them to choose between rent and prescription drugs.”
In the lawsuit, the attorneys general argue that the HHS and CMS rule is arbitrary and capricious, and contrary to law, in violation of the Administrative Procedure Act (APA). The coalition is also seeking preliminary relief, and a stay, to prevent the challenged portions of the final rule from taking effect in the plaintiff states before the effective date of August 25.
Congress enacted the ACA in 2010 to increase the number of Americans with health insurance and decrease the cost of healthcare. Fifteen years later, the Act continues to meet its goals, with annual enrollment on the ACA marketplace doubling over the past five years, resulting in over 24 million people signing up for health insurance coverage in plan year 2025 on the ACA exchanges and receiving subsidies to make such coverage affordable, including millions of people in the plaintiff states.
With less than four months until open enrollment for plan year 2026 begins, the Trump administration’s final rule would abruptly reverse that trend, erecting a series of new barriers to enrollment that will deprive up to 1.8 million people of insurance coverage and significantly drive up the healthcare costs incurred by plaintiff states, including increasing state expenditures on Medicaid, uncompensated emergency care, and funding for other services provided to newly uninsured residents.
Maryland has operated the Maryland Health Benefit Exchange since 2011, which has helped to cut in half the percentage of uninsured residents in the State, from 12% to 6%. The Exchange provides a robust market of choices for state residents, and its innovative policies have reduced individual market premiums by 30% since 2019.
But HHS’ final rule threatens this progress in making substantial changes and erecting bureaucratic barriers to the operation of the ACA marketplaces, including adding new verification requirements, imposing a monthly charge on all automatically reenrolled consumers who qualify for $0 premiums, shortening the open enrollment period for signing up for health coverage, and making other changes that will make coverage less affordable for millions of individuals nationwide.
These changes could lead up to 14% of enrollees on the Exchange, or 34,000 individuals, to lose coverage, while depriving Maryland of $4 million in lost revenue. And the increased paperwork requirements for enrollees and the Exchange will likely push additional younger and healthier individuals out of the marketplace, increasing premiums for the enrollees who remain, while significantly increasing costs and resource expenditures for the state.
The final rule would also exclude gender-affirming care as an EHB on federal exchange plans, leaving states responsible for paying for the portion of insurance premiums attributable to any such coverage.
In filing the lawsuit, Attorney General Brown joins the attorneys general of Arizona, California, Colorado, Connecticut, Delaware, Illinois, Massachusetts, Maine, Michigan, Minnesota, Nevada, New Mexico, New Jersey, New York, Oregon, Rhode Island, Vermont, Washington, and Wisconsin, as well as Pennsylvania Governor Josh Shapiro, on behalf of the Commonwealth of Pennsylvania.”